Leptin Could Revolutionise Treatment for Type 1 Diabetes

Leptin Could Revolutionise Treatment for Type 1 Diabetes
A UW study suggests leptin may offer new treatments for Type 1 diabetes, challenging long-held views on diabetic ketoacidosis.
A new study conducted by researchers at the University of Washington (UW) Diabetes Institute indicates that diabetic ketoacidosis (DKA), a severe complication associated with Type 1 diabetes, may be effectively treated by administering the hormone leptin. The findings, published in The Journal of Clinical Investigation, suggest a paradigm shift in understanding DKA, proposing that it may also be influenced by the brain’s perception of energy levels, rather than solely by insulin deficiency.
New Insights into Diabetic Ketoacidosis
DKA occurs when the body cannot produce insulin, prompting it to break down fat for energy. This process can lead to dangerously high levels of glucose and ketoacids in the bloodstream. According to Michael Schwartz, MD, a professor at the University of Washington School of Medicine, the research challenges the long-standing notion that insulin deficiency is the only cause of DKA. “This new framework shows that the brain plays a powerful role in the genesis of uncontrolled diabetes—and may hold the key to new treatments,” he stated.
The hormone leptin, which is produced by fat cells, helps regulate appetite and body weight by signalling sufficient energy stores to the brain. During periods of low insulin, as seen in uncontrolled Type 1 diabetes, leptin levels drop. This reduction leads the brain to incorrectly interpret the body as being energy-depleted, consequently triggering responses that exacerbate metabolic issues.
Recap of Previous Studies
This latest analysis builds on earlier research by Schwartz and his team from 2011, where they observed that administering leptin directly into the brains of rodents with uncontrolled Type 1 diabetes led to a swift normalisation of blood glucose and ketone levels, despite severe insulin deficiency. “The blood sugars just didn’t come down, but that the levels stayed down,” Schwartz remarked, referring to the lasting effects observed.
The findings from 2011 faced initial scepticism as they conflicted with prevailing theories regarding diabetes management. However, the current study provides a clearer understanding of the mechanisms involved.
Understanding Leptin's Role
The recent research highlights how the brain interprets signals from leptin and how this relates to DKA. When fasting or experiencing insulin deficiency, leptin levels drop sharply, signalling to the brain that fuel is scarce, even when the body is not actually energy-depleted. This miscommunication stimulates specific neural circuits in the brain that increase hormone secretion and contribute to elevated ketone production.
Through their research, the team discovered that restoring leptin recognition in critical brain areas or inhibiting certain neurons could reverse DKA in rodent models. “These observations reveal that the severe metabolic consequences of uncontrolled diabetes can be mitigated by convincing the brain that fuel reserves aren’t depleted,” the researchers noted.
Future Treatment Possibilities
While these findings offer a new avenue for DKA treatment, it is important to note that directly administering leptin into the brain is not a viable option for human patients at this time. The researchers did mention, however, that simply normalising peripheral leptin levels is inadequate for managing blood glucose but can help lessen the severity of ketosis.
There is hope that advancements in drug delivery methods could soon make it feasible to deliver leptin directly into the brain non-invasively. Irl Hirsch, MD, a co-author of the study, expressed optimism about these developments: “This is one of the most exciting discoveries of my career. This might be a better way.”
Next Steps for Clinical Trials
Schwartz and his team are now focused on seeking approval from the U.S. Food and Drug Administration (FDA) to initiate human trials aimed at determining if pharmacological leptin could normalise glucose levels in individuals with Type 1 diabetes. Should these trials succeed, they could shift the paradigm of Type 1 diabetes treatment from reliance on insulin to approaches that alter how the brain interprets metabolic signals.
“I think if you could treat Type 1 diabetes without daily insulin injections and blood sugar monitoring, patients would say that is the greatest thing ever,” Schwartz concluded.

India's Niti Aayog Proposes National EV Policy for 30% Sales by 2030
Niti Aayog calls for a national electric vehicle policy as India aims for 30% EV sales share by 2030, highlighting significant challenges ahead.
| 2025-08-05
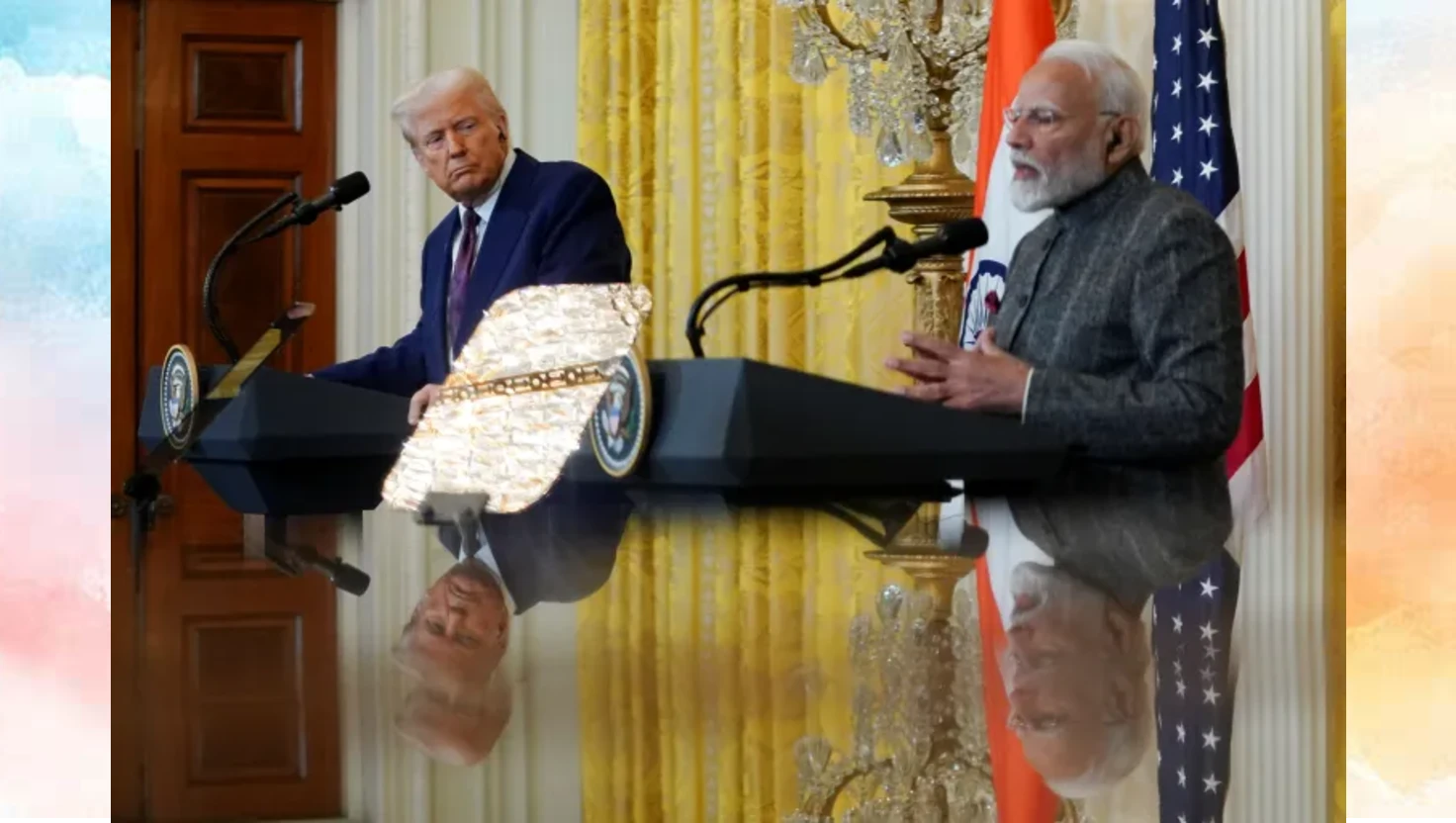
Trump says he will ‘substantially’ raise tariffs on India over Russian oil buys
Donald Trump announces plans to raise tariffs on India in response to its purchases of Russian oil, prompting a strong reaction from New Delhi.
| 2025-08-05

Philippine President Ferdinand Marcos Jr. Visits India for Talks
Philippines President Ferdinand Marcos Jr. embarks on a five-day visit to India to enhance bilateral relations and discuss cooperation across multiple sectors.
| 2025-08-05

Kremlin Downplays Trump's Nuclear Submarine Orders amid Tensions
The Kremlin has responded to US President Trump's nuclear submarine orders, advising caution in nuclear rhetoric during rising geopolitical tensions.
| 2025-08-05

Tesla Opens First Supercharger Station in Mumbai
Tesla inaugurates its first Supercharger station in Mumbai, marking a key milestone for electric vehicles in India, alongside the launch of Model Y.
| 2025-08-05




